The success of the rollout of COVID-19 vaccines in long-term care facilities is becoming apparent by the week, as COVID-19 cases among residents were — as of February 28 — the lowest they have been since May of last year.
Occupancy, though not rising remotely in proportion to the decline in new cases, has started to inch upwards, according to a new round of skilled nursing occupancy data from the professional services firm CliftonLarsonAllen (CLA).
National median occupancy for SNFs came in at 69.7% as of the end of February, compared with 69.2% at the end of January, and several states have begun to see even higher upticks. In West Virginia, for instance, median SNF occupancy rose 6.5 percentage points between January 3 and February 28.
“Nationally speaking, signs are continuing to support the bottom of occupancy was hit at the end of 2020, and we are in the turn,” Stephen Taylor, principal and CLA’s senior living segment leader, and CLA director Seth Wilson wrote. “So the question is: do we get back to our baseline (pre-COVID) operational reality; median operating margin of 0.0% and median
national occupancy of 84.6% … or do we have a new operational reality?”
CLA draws from the data skilled nursing facilities are required to report weekly to the Centers for Medicare & Medicaid Services (CMS) and the Centers for Disease Control and Prevention (CDC) for its analyses.
At the start of 2021, CLA found that all 48 of the continental United States had occupancy under 80%, with New York leading the way at 79%. In contrast, the most recent update found West Virginia leading states for median occupancy at 84.5%, followed by North Dakota at 80.5% and New York at 79.6%.
Oklahoma and Texas came in with the lowest median occupancies for their SNFs, at 55.8% and 55.9% respectively.
In its most recent update, CLA focused on the data around staffing and staffing shortages, an issue of increasing prominence for regulators and a long-standing problem for operators. In a recent Senate hearing, staffing shortages emerged as one of the most common aggravating factors in poor SNF care generally; shortages can also be a factor in COVID-19 outcomes, as there appears to be a connection between shortages and how an outbreak spreads.
In a recent set of policy proposals, the two largest trade groups for nursing homes — the American Health Care Association (AHCA) and LeadingAge — called for bolstering registered nurse (RN) coverage in nursing homes and establishing a strategy to address chronic workforce shortages in the long-term care field, where turnover can be 94% or higher.
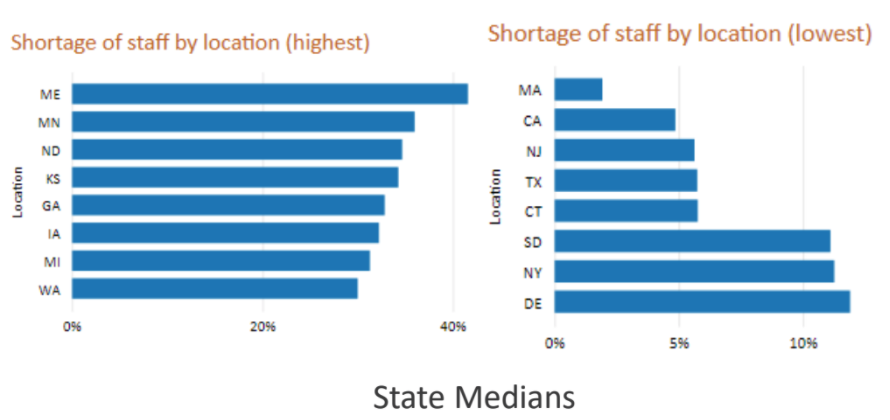
CLA found that approximately 20% of SNFs have reported a shortage of nurses or aides since June of last year; that represents the national median. By states, the shortages vary considerably; over 40% of facilities in Maine reported a shortage by the end of February, and unlike other states, the shortages seemed to be getting worse. Maine went from 31.2% of facilities reporting shortages on November 1, 2020, to 41.6% reporting shortages by the end of February.
In the state of Washington, 33.8% of facilities were reporting a shortage of nurses and aides on November 1, 2020, a number that rose just past 40% by the end of that month. But by the end of February, just 30% of facilities in Washington were reporting a staffing shortage.
The states with the lowest percentage of facilities reporting shortages were, in order from lowest to highest: Massachusetts, California, New Jersey, Texas, Connecticut, South Dakota, New York and Delaware.
The last three states still had more than 10% of facilities reporting a shortage, and New Jersey, Texas, and Connecticut still had more than 5% of facilities reporting shortages of staff.
The states with the highest percentage of facilities reporting staff shortages included, in order of highest to lowest: Maine with the most, followed by Minnesota, North Dakota, Kansas, Georgia, Iowa, Michigan, and Washington.
 CLA
CLA“Washington is an interesting case, as it has a staffing mandate that for some facilities may minimize the subjectivity from the definition of shortage,” Taylor and Wilson noted.



