Long-term acute care (LTAC) hospitals proved themselves a critical part of the public health response to the COVID-19 pandemic while also gaining a share of the patients discharged to facility-based care by short-term acute hospitals — even as the share of those patients going to the skilled nursing setting declined.
A new report, published February 15 by the Washington, D.C.-based consulting firm ATI Advisory, found that hospital discharges to LTACs and SNFs have fallen significantly overall, the result of “significantly lower” patient volume over the course of the public health emergency for the hospitals themselves.
In May 2020, discharges from hospitals fell 30% year-over-year; in turn, their discharges to LTACs dropped 34% year-over-year, while hospital discharges to the SNF setting declined 44%.
Bypassing SNFs after hospital stays has emerged as one of the many pain points for the sector during the pandemic; one analysis from the consulting firm Avalere Health found that the decline in Medicare hospital discharges to SNFs was “drastic and lasting,” compared to such discharges going to the home health setting. A different analysis from ATI Advisory on the Medicare data, published in November 2020, found similarly bleak results for SNF referrals from the hospital setting.
The February report on the role of LTACs highlighted how these facilities played a key part in the response to COVID-19 — most clearly by helping short-term acute care hospitals cope with patient surges, whether those patients had COVID-19 or not.
Because elective surgeries were canceled in the early months of the pandemic, the patient population overall tended to be sicker and more clinically complex, Tyler Cromer, a principal at ATI Advisory, noted in a Tuesday interview.
It’s not clear, however, whether the rise of LTACs and inpatient rehabilitation facilities will mean for SNFs. For one thing, the data is early — covering Medicare FFS claims data from January 2019 through May 2020 and paid through June of 2020 — so it only reflects the first three months of the pandemic.
For another, the complexity of patients might be a factor in why the share of hospital discharges to LTACs and IRFs rose in April and May 2020 from the same months in 2019, Conner Esworthy, an advisor at ATI Advisory, said in the same interview.
“It’s an overall more complex patient population,” she said, though she did note that this assessment was based on both case mix index and qualitative feedback from case managers and hospitals. “So one argument could be that these patients aren’t appropriate for SNFs. … You could say that LTACs and IRFs are filling this gap for SNFs because they’re potentially unable to take these patients — the patients wouldn’t be appropriate for these facilities anyway, because they are increasingly more critical.”
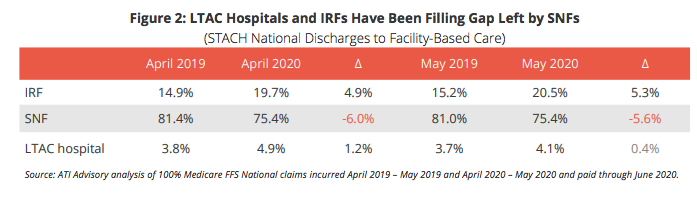
From April 2019 to April 2020, the share of patients discharged from hospitals who went to IRFs rose 4.9% year-over-year, while the share of patients discharged from hospitals who went to SNFs dropped 6% year-over-year. The share of hospital discharges going to LTACs, meanwhile, rose 1.2% in the same time frame.
From May 2019 to May 2020, the share of patients discharged from hospitals who went to IRFs rose 5.3%, while the share of patients from the hospital who went to the SNF setting dropped 5.6%, according to ATI Advisory.
“Prior to the PHE [public health emergency], and as a result of public policy and other legal restrictions, LTAC hospitals played a relatively narrow role in the health care delivery system; serving patients who had previously been in an intensive care unit or required mechanical ventilation,” the report noted.
Over the course of the pandemic, it appears that LTACs strengthened their partnerships with hospitals as they tried to handle the surge of both COVID-19 and non-COVID-19 patients, the report found, pointing to interviews with health care professionals and clinicians on top of the data analysis.
Their role could be summarized in four major themes:
- Government action waiving payment barriers and providing funding support that allowed faster care transitions
- LTACs serving an increasingly complex patient population over the course of COVID-19
- LTACs bolstering strategies to serve patients positive for COVID-19
- Changes in the ways LTACs and their capabilities are viewed over the course of the pandemic.
The ATI Advisory report also noted that managed care companies have taken notice of what LTACs can do. Much as SNFs have to wrangle with the prior authorization requirements of managed care companies, LTACs also deal with those regulations. But over the course of the pandemic, many managed care entities waived their prior authorization requirements, which allowed flexible care pathways for hospitals.
And though many plans have reinstated their prior authorization requirements, the claims data from the public health emergency could end up shedding light on how health plans’ discharge requirements affect care outcomes, the report noted.
“[Average length of stay] is very important,” a vice president of population health management at a managed care plan told ATI Advisory. “If a patient is going to a SNF, but staying 45 days and would have only stayed 20 in the LTAC hospital and then gets discharged home, that’s probably a better outcome.”
Kindred Healthcare, the former nursing home heavyweight that now focuses on higher-end settings such as LTACs and IRFs, welcomed the report in a Tuesday statement.
“Today’s ATI Advisory report underscores the unique value that LTAC hospitals bring to the nation’s most medically complex patients, and the solutions that they continue to deliver to patients and hospital partners throughout the public health emergency,” Kindred CEO Benjamin Breier said in the statement.
Kindred isn’t alone in seeing opportunity in the referral trends: Encompass Health Corporation (NYSE: EHC) as early as last summer positioned its IRFs as a better alternative to COVID-swamped SNFs.
“From a post-acute perspective, the patients that we’re treating in our IRFs really cannot go directly home from the hospital,” Encompass CEO Mark Tarr said last July. “They require an inpatient stay. So those patients, it becomes a choice between an IRF and SNF in almost all cases — and I would ask you for your opinion as to how the skilled nursing facilities have distinguished themselves during this pandemic.”


