For one skilled nursing operator in the greater Chicago area, success in the world of accountable care organizations has meant education and proactive collaboration — as well as a willingness to drop out of a partnership with an ACO that didn’t fit into its overall philosophy.
“We really look for a partnership in the ACO, but some ACOs have really more of a dictatorship,” John Vrba, CEO of Burgess Square Healthcare and Rehabilitation Centre, said during a Tuesday presentation at the American Health Care Association’s annual convention and expo in Orlando, Fla.
ACOs occupy a contentious place in the landscape of alternative payment models, with divided opinions on their overall efficacy — and a widespread perception that that many groups seek to cut costs by aggressively reducing lengths of stay at skilled nursing facilities.
In fact, that dynamic directly led Burgess Square, located in Westmont, Ill. to stop participating in one of its ACO partnerships. The SNF’s discharge team felt pressure to send one particular resident home earlier than they would have without the ACO, Vrba said, leading to a fall incident.
“It was a better move for our facility,” Vrba said. “We want to work with the ones that truly care, and truly have partnerships.”
That’s in contrast with another one of the company’s ACO collaborations, which Burgess Square administrator Kristin Thrun described as progressive — as opposed to aggressive.
“It’s not without its challenges, but our one ACO recognizes that they know nothing about SNF,” Thrun said. “They actually want to try to understand and work together to create processes that will work both in the SNF and in the hospital.”
Some of that work has included streamlining the internal ACO processes and paperwork. Each organization comes to the skilled nursing facility with its own set of standards and strategies, which can be confusing for an already overwhelmed administrative and caregiving staffs at both hospitals and SNFs, Thrun noted.
But the best ACOs will take the feedback, as long as SNFs are quick to provide it: For instance, Burgess Square’s complaints about inadequate medication-management information from its hospital partners prompted the ACO to step in and drive changes across the continuum.
“We didn’t have that same power,” Thrun said. “That’s really been a positive thing for us.”
Vrba has also begun preaching a move away from the term “length of stay” when dealing with ACOs, instead preferring “length of need” — hammering home that the SNF isn’t looking for extra days for purely financial reasons, but because the residents truly need more time before they can safely return home.
“We really have to rid ourselves, as a profession, of that terminology,” he said. “It’s really about length of need.”
In general, ACOs work by encouraging all of the providers along a single care episode — from the physicians to the hospital to the post-acute operators — to collaborate and find ways to reduce Medicare spending. Should they succeed, the Centers for Medicare & Medicaid Services (CMS) rewards the providers with a bonus, with penalties for ACOs that fail to produce savings.
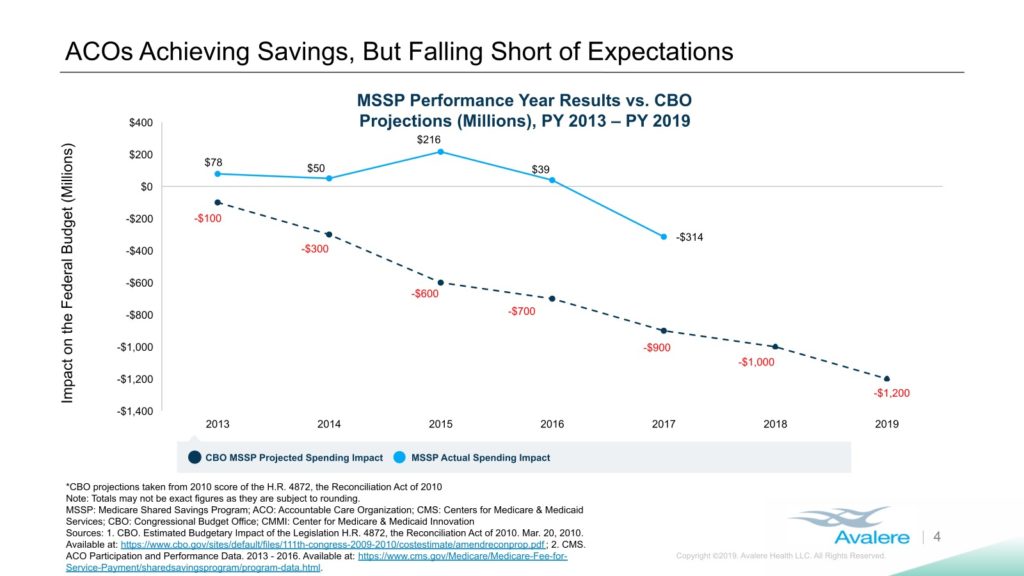
The program has evolved since its 2012 implementation, including the removal of bonus-only tracks, and the early returns have been mixed. Consulting firm Avalere Health, for instance, has produced research showing that the model has saved the government less money than initially projected.
What’s more, Avalere’s results indicate that ACO success may largely a matter of timing, with organizations typically only generating savings after their third year in operation.
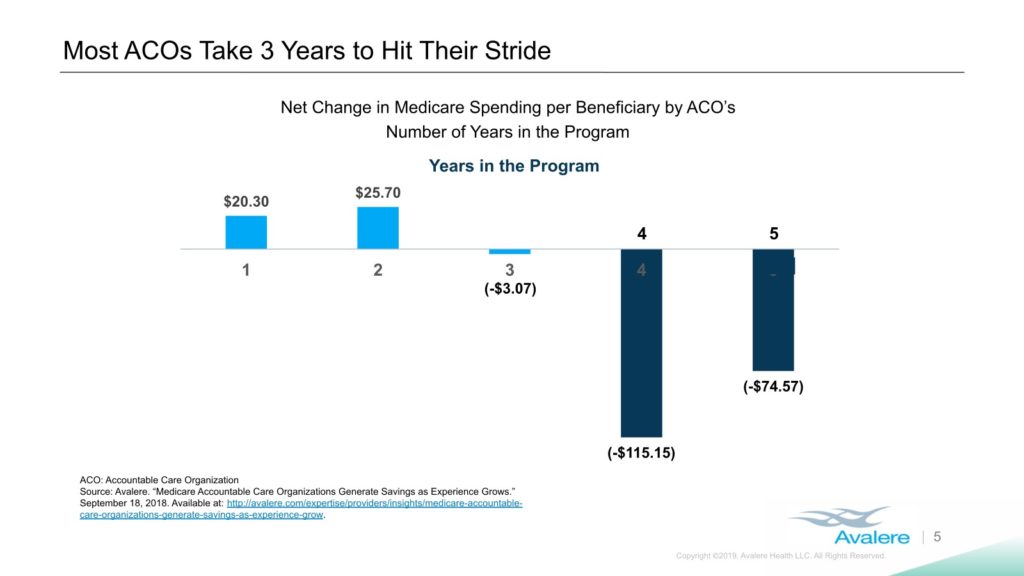
“ACOs do have an impact,” Avalere managing director Fred Bentley said during the presentation. “It’s incremental, not transformational.”
Avalere has previously pegged the total ACO-related loss to the government at $384 million between 2013 and 2016, the first three full years of the program; the federal government had predicted savings of $1.7 billon over that span. The National Association of ACOs, a Washington, D.C.-based trade group, has claimed actual ACO savings of $2.7 billion over that period, citing a different method of calculation.
“While true, looking at ACO performance compared to CMS-set spending targets is an overly simplified, wrong way to judge ACOs,” David Pittman, health policy and communications advisor for NAACOS, told SNN in an e-mail earlier this year. “It doesn’t compare what Medicare spending would be like in the absence of ACOs. This method shows large savings driving by ACOs.”
No matter the overall stats, skilled nursing facilities have been firmly in ACOs’ crosshairs, with multiple studies showing that reductions in SNF usage have helped to fuel overall Medicare savings. One anonymous skilled nursing operator went so far as to call the program a “disaster” for the industry in an interview with SNN.
But the goal of achieving ACO savings may not be quite that simple. Citing new research that Avalere has not yet released, Bentley said that reducing hospital admissions may have a stronger impact than cutting out SNFs.
“The ACOs that really succeed, it’s not that they’re coming after SNFs — although some of them are, and they will be, and certainly have been,” Bentley said. “The big success factor is driving down hospitalizations.”
And the ACOs that truly succeed at that metric are those led by physician groups, and not hospitals, according to Bentley. While hospitals have traditional pressure to maintain their own census and keep “heads in beds,” physicians have no such concerns, and can thus target costly acute stays as a key driver of savings.
“Physician groups don’t have that legacy inpatient footprint,” he said. “They don’t have to be concerned with that, so they are targeting hospitalizations.”
That trend doesn’t necessarily spell happy days for nursing homes; a decline in hospital visits could potentially have a trickle-down effect on post-acute care utilization that would still result in lower Medicare reimbursements for SNFs. But the main takeaway, at least in Bentley’s view, is that the ACO model is constantly changing — and any effects, positive or negative, could take years to fully appear.
“They were presented as the savior, this brand new model that was really going to transform health care and usher in this move to value-based care,” Bentley said of the program. “That’s not true.”
Companies featured in this article:
American Health Care Association, Avalere Health, Burgess Square Healthcare and Rehabilitation Centre



