The gulf between self-reported and payroll-based staffing records for nursing homes continues to widen, with a new study showing a reality that vastly differs from government expectations.
The amount of registered nurse (RN) coverage falls well below the standards set by the Centers for Medicare & Medicaid Services for most skilled nursing facilities in the country, a team from Harvard and Vanderbilt University reported in a study published Monday in the July issue of the journal Health Affairs.
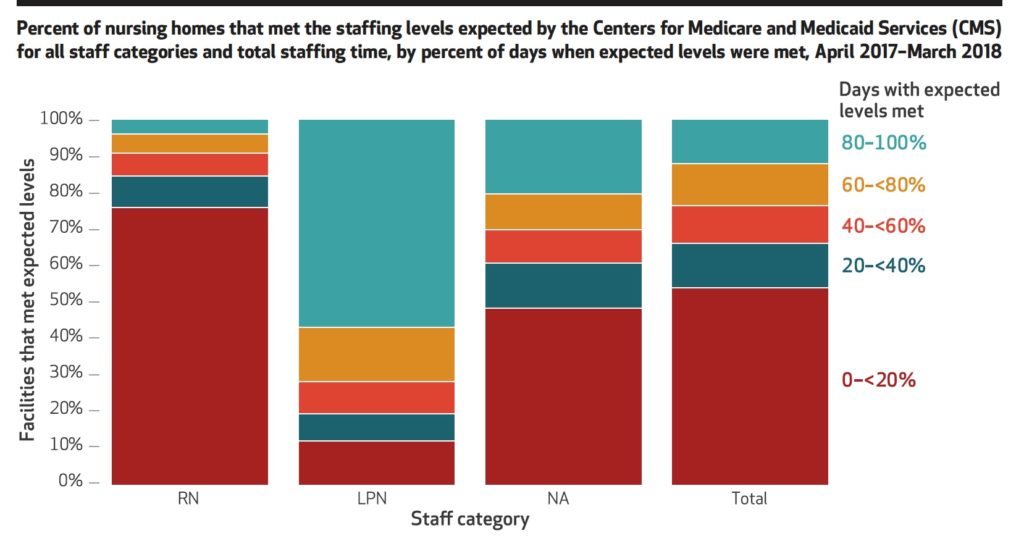
“One troubling aspect of our findings is that 75% of nursing homes were almost never in compliance with what CMS expected their RN staffing level to be, based on residents’ acuity,” the authors — Fangli Geng, David Stevenson, and David Grabowski — wrote.
While operators performed slightly better with licensed practical nurse (LPN) coverage, about half of the country’s SNFs only met expected benchmarks for overall staffing on 19 days or fewer between April 2017 and March 2018.
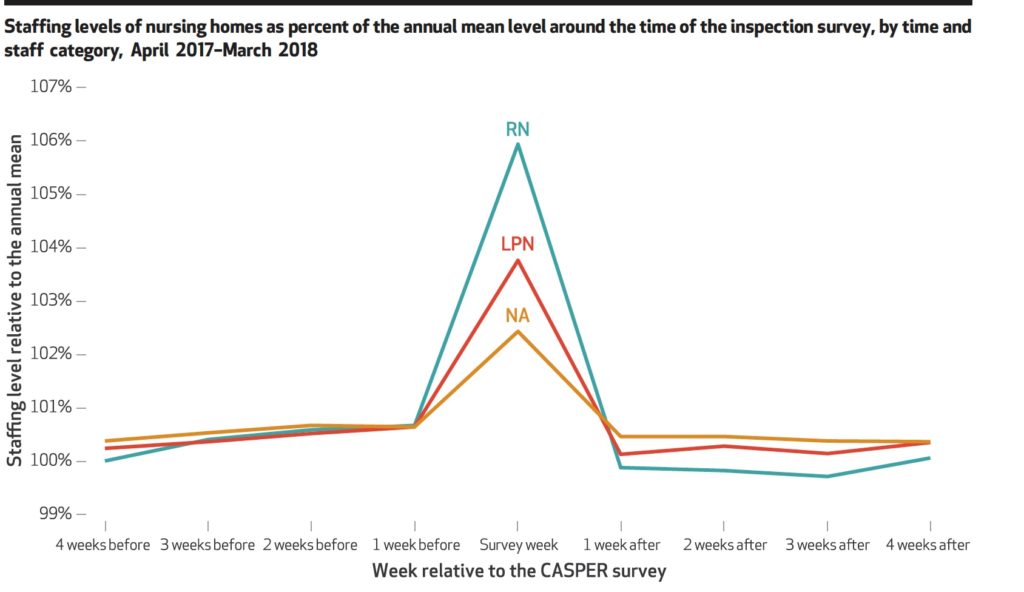
In addition, the Harvard-Vanderbilt team confirmed a trend that had long been observed and discussed on an anecdotal basis: staff levels peaking right around the time of the facility’s annual survey.
“In the weeks before and after the survey week, mean staffing levels were higher than annual staffing levels,” the researchers concluded. “Staffing levels increased before the survey week, reached a peak during the survey week, and then dropped following the survey. Trends were consistent across staffing categories (RN, LPN, and nurse aide), but RN staffing had the largest increase around the time of the survey.”
The study adds to an already robust analysis of potentially troubling staffing patterns in nursing homes, particularly after CMS switched from self-reported data to the payroll-based journal (PBJ) system in April 2018.
The New York Times and Kaiser Health News last summer raised the alarm about SNFs over-reporting their actual staffing levels after analyzing the first round of PBJ data; in response, CMS slapped nearly 1,400 nursing homes with one-star staffing ratings last July, and rolled out new stricter staffing standards in an overhaul of the five-star rating system for facilities this past spring.
That said, the Harvard-Vanderbilt researchers found some bright spots in the numbers — though they concluded that the metrics themselves might need overhauling to truly present an accurate picture of staffing issues.
“Almost all nursing homes met the federal eight-hour RN staffing requirement for the majority of days,” they wrote. “These conflicting results suggest that the eight-hour requirement does little to ensure adequate RN staffing levels needed to care for people who live in nursing homes.”
Researcher Grabowski, who also sits on the Medicare Payment Advisory Commission (MedPAC), generally praised CMS’s efforts, but identified a few areas where he thinks the federal government should further bolster nursing home workforce information — specifically around night and weekend staffing, which his team found was substantially lower than during weekday business hours.
“More measures that are based on the day-to-day variation, rather than a simple average, I think would really help consumers,” Grabowski told SNN. “I do care about the average. It’s informative, but I care what happens to my mom on that Wednesday afternoon when they were understaffed.”
Moving forward, Grabowski said he hopes CMS will continue to use the PBJ data to provide more clarity to consumers about actual nursing home staffing — while also providing a pathway for officials to monitor and punish those that fall short of the mark.
“I do think at their core, they get at low staffing,” Grabowski said of CMS. “Staffing is the most important input into strong quality of care.”


