A new federal report on nursing home deficiency trends saw an up-and-down pattern in recent years, with a handful of states generating the lion’s share of issues.
Officials at the Department of Health and Human Services (HHS) Office of the Inspector General (OIG) found the number of nursing home surveys and deficiencies rose slightly each year from 2013 to 2016, and then slightly fell in 2017. Ten states accounted for 50% of the deficiencies identified, while the top 10 of 340 deficiency types accounted for more than 40% of deficiencies.
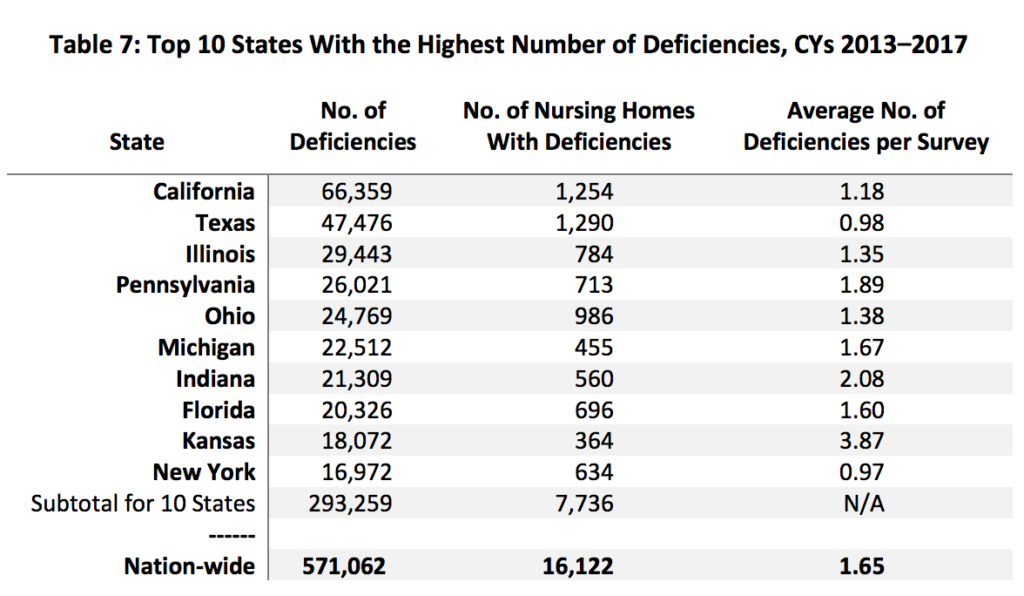
Those states track loosely with the states with the highest number of nursing facilities, according to 2016 data from the Kaiser Family Foundation (KFF). In that data set, Texas ranked No. 1 with 1,220 facilities, and California followed with 1,203. Ohio, Illinois, Pennsylvania, Florida, New York, Indiana, Missouri and Michigan rounded out the top 10 states, respectively.
The OIG report tracked both the number of available surveys and deficiencies, with surveys ranging from 64,500 to 72,900 each year — while deficiencies identified ranged from 108,600 to 120,900 each year.
From 2016 to 2017, the number of deficiencies fell slightly, from 120,900 to 116,000; the number of surveys also dropped slightly, from 72,900 to 70,400.
But one encouraging aspect was that 94% of deficiencies were identified as “less serious;” more than 100,000 less serious deficiencies were identified per year, while more serious ones came in at an average of 7,100 a year.
About 31% of SNFs had a repeat deficiency, and the states with the highest percentages of SNFs with at least one repeat deficiency were Washington D.C., Maryland, Connecticut, Washington state, and Delaware. Massachusetts, New Hampshire, Georgia, Hawaii, and Rhode Island had the lowest percentage of nursing homes with at least one repeat deficiency.
In a previous report, the OIG found seven of nine state agencies did not always verify SNFs’ correction of deficiencies, as is required, and that combined with the new findings suggests that SNFs may be falling short in making changes to prevent deficiencies, the agency said.
“The findings from our previous report and our data analysis for this data brief suggest that nursing homes may not have been properly implementing systemic changes to ensure that deficiencies do not recur,” the report said.
To compile its new report, the OIG reviewed nursing home deficiencies identified by state survey agencies across the U.S. for calendar years 2013 through 2017. The OIG primarily used data from the Centers for Medicare & Medicaid Services’ (CMS) Certification and Survey Provider Enhanced Reporting (CASPER) system, also drawing from Minimum Data Set (MDS) reports from the CMS website — but the analysis had some limitations, the OIG noted.
“[O]ur data analysis did not account for possible variations in how state agencies conducted surveys and identified noncompliance with Federal participation requirements,” the OIG wrote in its report. “Finally, we did not address any underlying reasons for changes in the data, such as changes to the ease of filing complaints or improvements in CMS’s surveyor guidance. These factors could have affected the number of deficiencies identified in each State.”
State-level surveys came under fire in a recent report from the U.S. Government Accountability Office, which found that CMS failed to adequately oversee state survey agencies in Oregon. The Beaver State’s Adult Protective Services (APS) unit was investigating complaints and facility-reported incidents of abuse in SNFs despite lack of training in investigating abuse under federal nursing home rules
Companies featured in this article:
Centers for Medicare & Medicaid Services, Department of Health and Human Services, Office of Inspector General


