Value-based programs can lead to lower costs of care and better quality of care for seniors enrolled in Medicare Advantage (MA) plans, according to an internal study from Louisville, Kentucky-based health insurance provider Humana.
The study found total health care costs for practices in Humana’s value-based arrangements were 15% lower than original fee-for-service Medicare. Compared with standard MA settings, total health care costs were 4% lower.
Standard Medicare Advantage plans do not offer additional incentives to providers who meet cost or quality targets.
“Fee-for-service is a fragmented system. It’s fragmented in the primary care world, it’s certainly fragmented in the specialty world and it’s certainly fragmented in the at-home world,” Dr. Roy Beveridge, Humana’s chief medical officer, told Skilled Nursing News.
The federal government provides Medicare Advantage plans with a set amount of money to provide benefits to their beneficiary population. The plans have considerable flexibility in managing and coordinating the care in order to make a profit while keeping up quality.
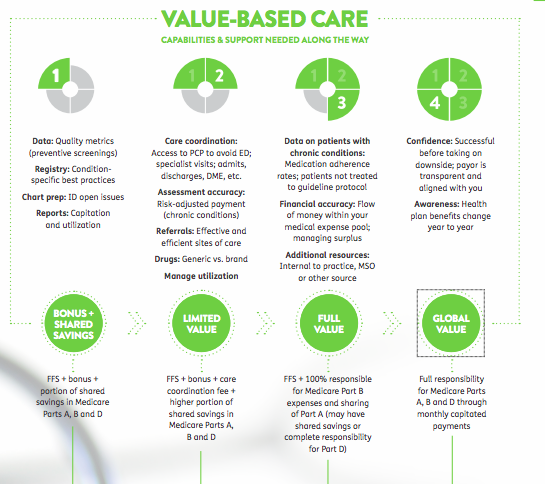
Humana’s report discussed three categories of payment — fee-for-service, bonus and value-based care — and covered four value-based payment models, which include more pay for meeting quality measures and preventing repetitive treatments, among other factors.
The study dealt more with primary care physicians than other kinds of providers, Beveridge indicated. But he noted that primary care doctors work with other providers, such as skilled nursing.
“What we’re trying to do is use our analytics to understand what’s happening with our patients and then coordinate with the home care company or any post-acute company… and to help with the coordination back to the doctor’s offices,” he explained.
The value-based care report looked at quality metrics and prevention measures in calendar year 2016 for about 1.65 million Humana MA members in value-based reimbursement model agreements, then compared those numbers with those for 191,000 Humana members linked to standard MA providers.
It also examined costs in the same timeframe for about 1.4 million Humana MA members connected with providers in value-based arrangements, comparing them to fee-for-service Medicare. In addition, it compared outcomes for those 1.4 million to results for 216,000 Humana members linked to providers in standard Medicare settings.
It found the doctors practicing value-based care obtained higher patient engagement rates in preventive screenings, chronic condition management and medication adherence, as measured by the Healthcare Effectiveness Data and Information Set (HEDIS). In fact, patients treated by doctors in Humana’s MA value-based agreements saw more preventive care screenings and better health outcomes, compared with patients in Humana MA fee-for-service agreements.
Making sure patients have the right medication is crucial for skilled nursing facilities, and Beveridge stressed the importance of proper medication for overall patient health.
“Frequently the patient has a shoebox for medicines and they just start taking them,” he said. “It’s incredibly dangerous. Up to a third of hospital readmissions may be due to incorrect medications.”
This highlights the importance of such steps as medication reconciliation in the nursing home, but Beveridge strongly encourages SNFs and other providers to think bigger. Humana, for instance, provides food for patients for up two to four weeks after discharge if they are food-insecure, or helps with transportation in certain areas, he noted. The goal is to care for the highest-cost patients, many of whom are under the sway of forces other than physical ailments.
“What we’ve found is that a lot of these things can be related to social determinants of health such as food insecurity,” he said.
Humana’s study could provide more evidence of the critical need for high-quality skilled care within a landscape that’s increasingly turning to the value-based system. For instance, the Skilled Nursing Facility Value-Based Purchasing Program (SNFVBP) from the Center for Medicare and Medicaid Services (CMS) is set to take effect in fiscal 2019, putting increased pressure on SNFS to plan for the the entire process of care: Under the new SNFVBP rules set to go into effect next October, skilled nursing operators will automatically lose 2% of their Medicare reimbursements, which they can earn back by reducing readmissions.
Written by Maggie Flynn



